
Let’s Bring Attention to IBS
If you are one of the estimated 25 to 45 million Americans who suffer from IBS, you will want to join Needham Gastroenterology Associates this April to bring attention to the disease for IBS Awareness Month. It’s important to speak up about the disease, understand the symptoms, and visit your doctor if you think you might have irritable bowel syndrome and haven’t been diagnosed.
What is IBS?
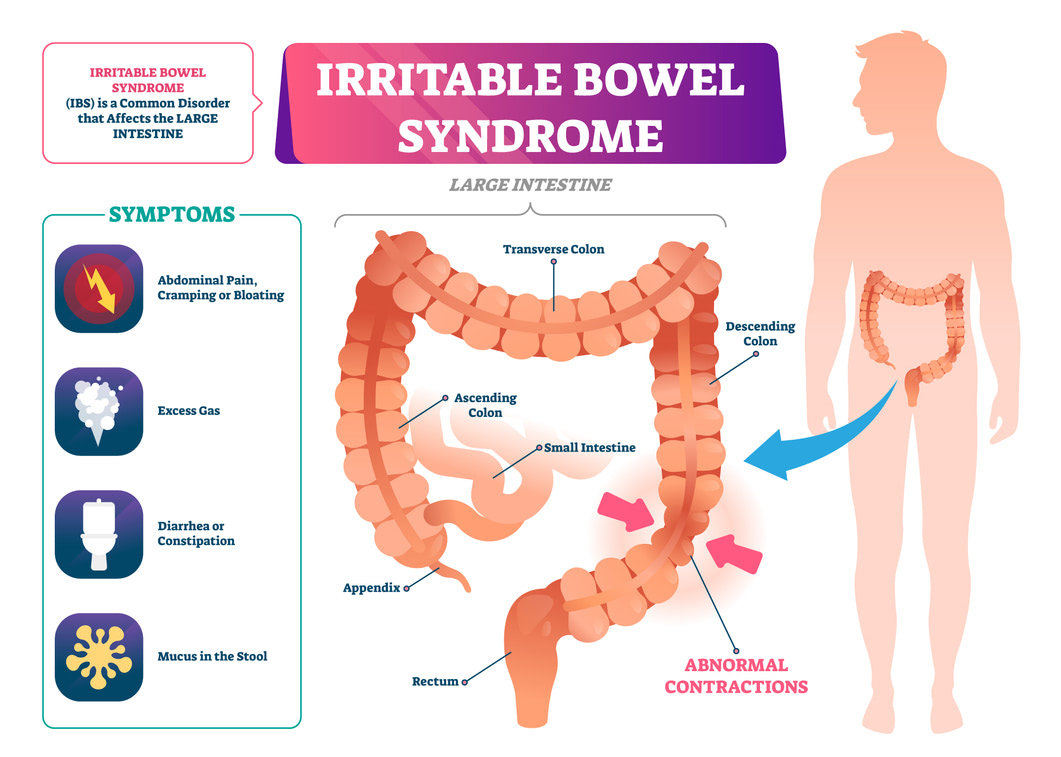
Understanding what the disease is, how it manifests itself, and what you can do about it once you’re diagnosed is the most important part of IBS awareness. IBS, or irritable bowel syndrome, affects the digestive tract and is characterized by pain and discomfort in the abdomen, as well as bowel habits including either diarrhea, constipation, or sometimes even a combination of both. Most IBS patients know they have the disease through a few common symptoms including persistent pain not relieved by passing gas or having a bowel movement, cramping, gas, pain in the abdomen, diarrhea or constipation, bleeding from the rectum, unintended weight loss, and bloating. IBS can present differently in different people, or even vary day to day depending on your diet and lifestyle. There is no blood test that can tell whether you have IBS, but doctors will take a full history and do a physical exam to determine a course of treatment. Since many GI illnesses can present with similar symptoms, we may also want to rule out something more serious. This can be done through physical exams including endoscopies, colonoscopies, X-rays or CT scans, stool test, or food allergy testing.
What Causes IBS? Why Do Symptoms Flare?
It might be frustrating to hear this, but nobody is totally sure what causes IBS. It’s thought that people who suffer from IBS might have a disconnect between the way their nervous system interacts with their brain and gut, meaning that the normal feelings you have when you need to have a bowel movement might be different in those with IBS when compared to people who don’t have the disease. Some symptoms can also be connected with stress, hormonal changes, certain antibiotics, or even brought on by an infection in the digestive tract. It is also more common to see in patients with a family history.
Different people might have a different severity of the disease, ranging from a small inconvenience to a debilitating problem that leaves you at home and never too far from a bathroom. While triggers may differ from person to person, they most often include food, stress, and hormones. The flare-ups may also change depending on different circumstances, meaning one day you might have diarrhea, followed by constipation.
How Can a Low-FODMAP Diet Help?
The foods that are causing your symptoms may be ones that you never would have considered, like apples or garlic. With the low-FODMAP diet, you can determine what foods trigger your IBS.
According to a study in PubMed, 76 percent of people with IBS who tried the low-FODMAP diet had a reduction in IBS symptoms. 82 percent saw a decrease in bloating. Flatulence, diarrhea, and constipation can also be significantly reduced with this diet.
John Hopkins Medicine explains it like this:
“Low FODMAP is a three-step elimination diet:
- First, you stop eating certain foods (high FODMAP foods).
- Next, you slowly reintroduce them to see which ones are troublesome.
- Once you identify the foods that cause symptoms, you can avoid or limit them while enjoying everything else worry-free.”
What Should My Next Steps Be?
If you think you might be suffering from IBS, make an appointment at Needham Gastroenterology Associates to discuss your symptoms and see if you could benefit from treatment possibly including a change in diet and lifestyle. Start keeping track of what you’re eating and how it affects you, as well as the severity of symptoms and if there is anything you can do to relieve them. This will help us understand how your symptoms present and how we can establish a routine that can help you feel better and keep your symptoms in check.