Don't Wait; Cirrhosis Of The Liver Is The Late Stage
Cirrhosis is a late-stage condition resulting from liver disease and its complications. In the beginning of the illness, you may not experience symptoms. Alcoholism, hepatitis, and non-alcoholic fatty liver disease are all examples of common causes. Treatment is determined by the cause of cirrhosis and how much harm has occurred. Let's learn more and how liver and cirrhosis can be gastro issues.
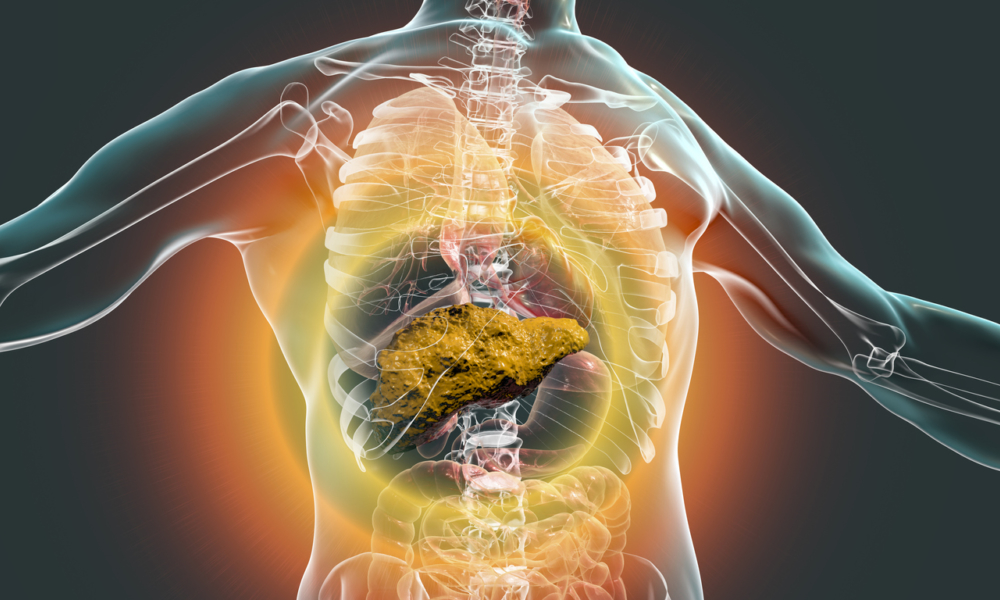
Liver Cirrhosis
Cirrhosis is the late-stage of liver disease in which the healthy tissue in your liver is replaced with scar tissue. This damages your liver and prevents it from working correctly.
When diseases or conditions injure healthy liver cells, they begin to die and become inflamed. This is followed by cell repair and tissue scarring resulting from the repair process.
The damage to the liver caused by alcohol is irreversible. The build-up of scar tissue obstructs blood flow and slows the liver's capacity to metabolize nutrients, hormones, medications, and natural poisons. It reduces the production of proteins and other molecules produced by the liver. Cirrhosis eventually prevents the liver from functioning effectively. Cirrhosis in its advanced stage is deadly.
Is cirrhosis common?
Cirrhosis of the liver is a problem that about 1 in 400 adults face in the United States. To give some perspective, this means that cirrhosis affects more people than suicide, which was the 10th leading cause of death in 2018. Cirrhosis also commonly manifests itself around age 45 to 54 and causes 26,000 deaths annually.
Who is most at risk for cirrhosis?
The following increases your chance of developing cirrhosis of the liver:
- Alcohol abuse
- Viral hepatitis
- Diabetes
- Obesity
- The use of shared needles to administer drugs
- If you have a family member who has had liver disease
- Unprotected relations
Cirrhosis is not an inherited disease; however, some conditions can cause liver damage and lead to cirrhosis.
Is cirrhosis reversible?
No. If you've been diagnosed with cirrhosis, you likely have late-stage liver disease, and the harm that has already been done is irreversible. There are numerous types of liver diseases and complications, some of which can cause cirrhosis. It's possible to slow or stop disease advancement if your liver illness or difficulty is identified early and effectively treated.
Is cirrhosis a death sentence?
While a diagnosis of liver cirrhosis doesn't immediately mean you will die, the condition gradually worsens as scarring increases and liver function declines. If left untreated, your failing liver could become fatal. But there is still hope: You and your doctor will determine if you qualify for a transplant, so you'll be placed on a national waiting list for a new organ.
Cirrhosis Symptoms
Cirrhosis has different symptoms depending on how far the disease has progressed. In the early stages, you might not experience any symptoms. If you have them, they tend to be general and could easily be blamed on other diseases or illnesses.
Early symptoms and signs of cirrhosis include:
- Appetite loss
- Fatigue
- Nausea
- Fever
- An unexpected loss of weight
Other symptoms of cirrhosis that may appear as liver function deteriorates include:
- Bruising and bleeding easily
- Jaundice
- Skin that becomes itchy
- Edema or swelling in legs, feet, and ankles
- Belly/abdomen fluid build-up (ascites)
- Urine that is brown or orange
- Pale-colored stool
- Confusion
- Blood in stool
- Palms that become red
- Telangiectasias (Spider-like blood vessels that surround small, red spots on your skin)
Cirrhosis Causes
Common causes of cirrhosis:
- Alcohol abuse
- Hepatitis B and Hepatitis C (Chronic viral infections of the liver)
- Fatty liver associated with diabetes and obesity (non-alcoholic steatohepatitis)
Cirrhosis is a gradual process caused by liver diseases. Liver cells are injured, and if the injury continues, they start to die. Scar tissue replaces the damaged liver cells, causing the liver to not function.
Diagnosis of cirrhosis of the liver?
A history of drug or alcohol abuse, hepatitis B or C, your healthcare provider will consider the possibility you have cirrhosis. Reviewing your medical history, current medications (prescription and over-the-counter), and any supplements or herbal products you take to reach this conclusion.
To diagnose cirrhosis, your provider will need to perform a physical exam as well as order at least one of the following tests:
- Physical exam: Your physician will examine you for signs and symptoms of cirrhosis, such as the appearance of red, spider-like blood vessels on your skin; yellowing of your skin or eyes; bruising on your skin; redness in your palms; swelling, soreness, or pain in your abdomen; and an enlarged, bumpy texture to the lower edge of your liver (the part of your liver below the rib cage that may be felt).
- Blood tests: Your physician may order blood tests to look for signs of liver disease if they suspect cirrhosis. The following are some of the indicators of liver damage:
- Lower-than-average levels of albumin and blood clotting factors in your liver could signify that it has lost its ability to produce these proteins.
- Higher than average levels of liver enzymes indicate potential inflammation.
- Vitamin B12 deficiency: Increased levels of iron (may indicate hemochromatosis).
- The presence of autoantibodies may be an indicator of autoimmune hepatitis or primary biliary cirrhosis.
- A bilirubin level that is too high suggests that the liver isn't working correctly to remove bilirubin from the blood.
- Increased white blood cell count (indicates infection).
- This suggests kidney disease and late-stage cirrhosis.
- Lower levels of sodium may indicate the presence of cirrhosis.
- Alpha-fetoprotein (a protein that is produced from the liver) has increased by a level of 13.8%. This is linked to the presence of liver cancer.
Other blood work could include a complete blood count to look for signs of infection or anemia. Or a viral hepatitis test to check for hepatitis B or C.
- Imaging tests: A computerized tomography (CT) scan, abdominal ultrasound, and magnetic resonance imaging (MRI) are all possible liver examination tests. These scans can also reveal scarring, fat accumulation in the liver, and fluid accumulation in your stomach. Magnetic resonance imaging (MRI, computerized tomography (CT) scan, and abdominal ultrasound are three types of liver examination tests that might be done. A special ultrasound, known as transient elastography, is used to assess liver fat content and degree of stiffness. An endoscopic retrograde cholangiopancreatography might be performed to look for bile duct issues, and an upper endoscopy to discover distended veins (varices) or bleeding in your esophagus, stomach, or intestine.
- Biopsy: A biopsy, or a sample of liver tissue (biopsy), is taken from your liver and examined under the microscope. A liver biopsy can determine whether you have cirrhosis, identify other causes of your liver damage, assess its severity, or diagnose liver cancer.
Stages of cirrhosis?
Although liver specialists and researchers have created multiple scoring systems to anticipate results and direct treatment for chronic liver disease, some specific diseases still don't have their systems. If a person has more than one liver condition simultaneously, no predetermined scoring method applies.
For these reasons, it may be simpler to discuss cirrhosis in terms of a categorization system that your healthcare provider is more likely to mention. They might call you compensated or decompensated cirrhosis.
Compensated cirrhosis If your doctor has discovered a focus (such as another liver disorder), he might order other tests to rule out any additional causes for the focus's presence. Many people aware of their condition may be unaware of the blood test that can diagnose it sooner. Positive results will show up on your test right away; however, adverse consequences take longer to appear because they are confirmed by a second test (titration) before they can be considered accurate.
Decompensated cirrhosis: decompensated cirrhosis is when your cirrhosis has worsened to the point where you have visible symptoms. Your healthcare practitioner will evaluate your situation based on your past physical and laboratory findings. You suffer at least one problem, such as jaundice, ascites, hepatic encephalopathy, hepatorenal syndrome, variceal bleeding, or liver cancer. For the most part, patients with decompensated cirrhosis are hospitalized for treatment. The median survival time for individuals with compensated cirrhosis is two years.
Does cirrhosis of the liver have a cure?
There is no cure for cirrhosis. The damage to your liver has already been irreversible. However, you may make efforts to prevent your cirrhosis from getting worse depending on the source of your cirrhosis. These measures include:
- Abstain from drinking alcohol
- Treat chronic hepatitis
- Avoid liver stressing medication
- Eat a healthy, well-balanced, low-fat diet
Cirrhosis Treatments
Treatment depends on your cirrhosis' cause and extent. Although there is no cure for cirrhosis, medicines can slow or stop its development and promote fewer problems.
Treatments of cirrhosis are as follows:
- Alcohol-related liver disease: If you have cirrhosis from alcohol abuse, you must stop drinking. If you are struggling to do so, reach out to your healthcare provider for help finding an alcohol addiction treatment program.
- Hepatitis B or C: Several antiviral medicines can be used to treat hepatitis B and C.
- Non-alcoholic fatty liver disease: Some tips for managing non-alcoholic fatty liver disease are losing weight, eating healthy foods, exercising regularly, and following your provider's instructions for managing your diabetes.
- Inherited liver diseases: The treatment for alpha-1 antitrypsin deficiency depends on the type of inherited illness. Treatments are focused on alleviating symptoms and managing side effects. Treatment for alpha-1 antitrypsin deficiency might include anti-inflammatory medications to reduce inflammation, antibiotics to treat infections, and other medicines to manage problems. For hemochromatosis, the treatment would be to remove blood to reduce iron levels. For Wilson's disease, copper-removing drugs and zinc are prescribed to prevent further absorption. As for cystic fibrosis, medications are given to help lung function better, and treatments to clear mucous and manage complications. Lastly, glycogen storage diseases require glucose maintenance at correct levels via liver care.
- Autoimmune hepatitis: To suppress your immune system, you must take certain medications as part of your treatment.
- Diseases that damage or block the bile ducts in the liver: Ursodiol (Actigall®) or surgery to open restricted or blocked bile ducts are used in treatments.
- Heart failure: The treatment for heart failure is determined by the cause and severity of your condition. Drugs that treat high blood pressure, reduce cholesterol levels, eliminate excessive bodily fluids (edema), and improve heart pumping are all used in therapy. Other procedures include implanting medical devices to assist pump blood or tracking heart rhythm, cardiac operations to unblock arteries or replace or mend heart valves, and transplant surgery to replace your entire organ.
Needham Gastroenterology Associates Can Help
Needham Gastroenterology Associate encourages you to contact us and set up an appointment for screening, diagnosis, and treatment. Remember your gut health affects more than just your digestion and to live a healthy life it can begin in the bowls.